Beyond The Hours Slept
Inconsistent Sleep Routines Threaten Mental Health In 100,000 UK Biobank Participants
BMC Public Health 2025Abstract
Background: Sleep duration has a well-established effect on mental health and well-being, with durations of 7 to 9 hours being the general recommendation. Here, we analyze the significance of sleep patterns and find that a consistent routine reduces the risk of developing mental disorders far more than simply ensuring a certain average sleep duration.
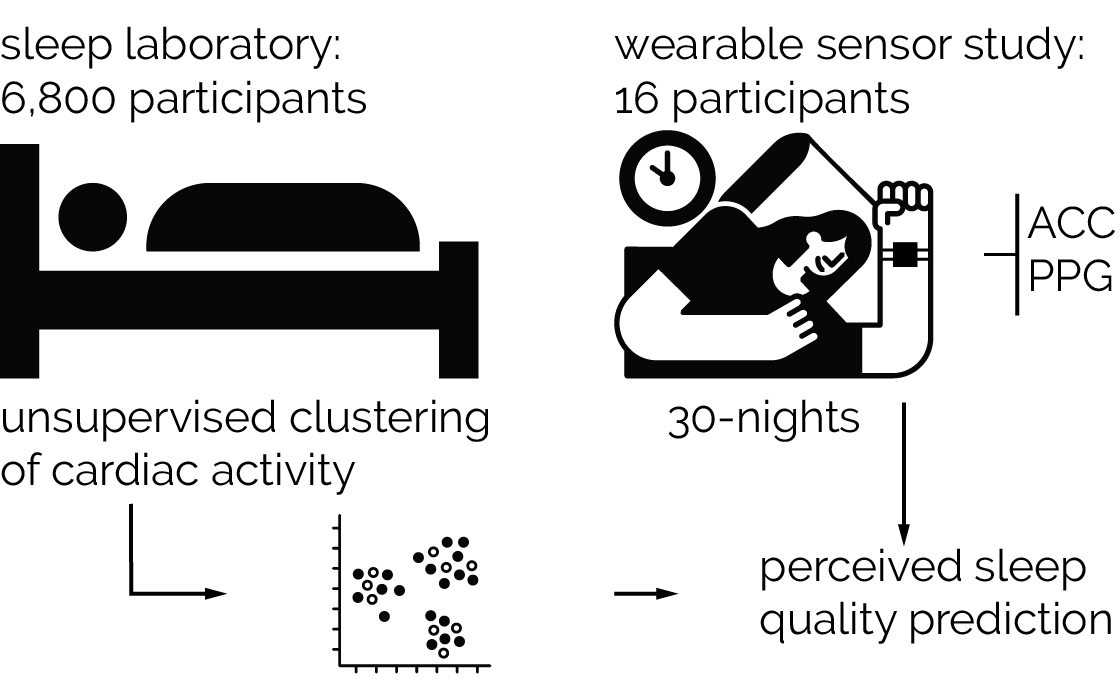
Methods: We analyzed the sleep behavior of 100,000 adults for one week using motion data from wrist-worn devices. We modeled sleep behavior using multivariate generalized additive Cox proportional hazard models, incorporating a smooth 2D interaction effect of sleep duration and routine sleep hours. We calculated C-statistics and E-values to evaluate model performance and assess the robustness against hidden confounders. We also stratified analyses by age and gender.
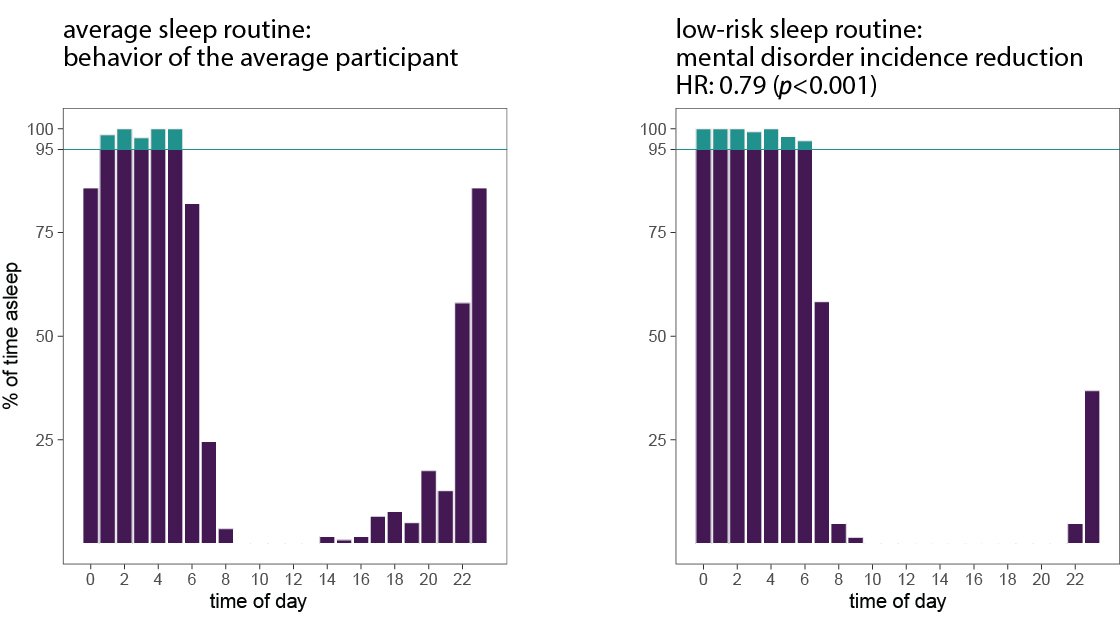
Results: Most participants slept for 7 to 9 hours as recommended, yet they consistently only slept during the same 4.8 hours each night. We found that an average sleep duration around 8 hours minimizes the risk of future mental disorders—but only if integrated into a rigorous sleep routine spanning at least the same 7 hours each night. Our study provides evidence that adopting such sleep behavior could reduce the population incidence rate of mental disorders by 23% (HR: 0.79, p < 0.0001, for the average participant). The models showed a strong fit (C-statistics: 0.63), robustness to hidden confounders (E-value: 1.8), and stability under age- and gender-based stratification. We identified weekend behavior as a frequent reason for low sleep routines, with over 25% of the population disrupting their weekly sleep routine during weekend nights—raising the risk of future mental disorders by 10%.
Conclusions: Our results suggest that maintaining a consistent sleep routine is more important for mental health than sleep duration alone. Socially disadvantaged groups, including low-income households and ethnic minorities, exhibited poorer sleep routines and thus higher mental disorder risks, underscoring existing social inequalities. Promoting regular sleep behavior may therefore have significant public health benefits.
Reference
Max Moebus and Christian Holz. Beyond The Hours Slept: Inconsistent Sleep Routines Threaten Mental Health In 100,000 UK Biobank Participants. In BMC Public Health 2025.
Divergence Between Sleep Duration And Sleep Routine
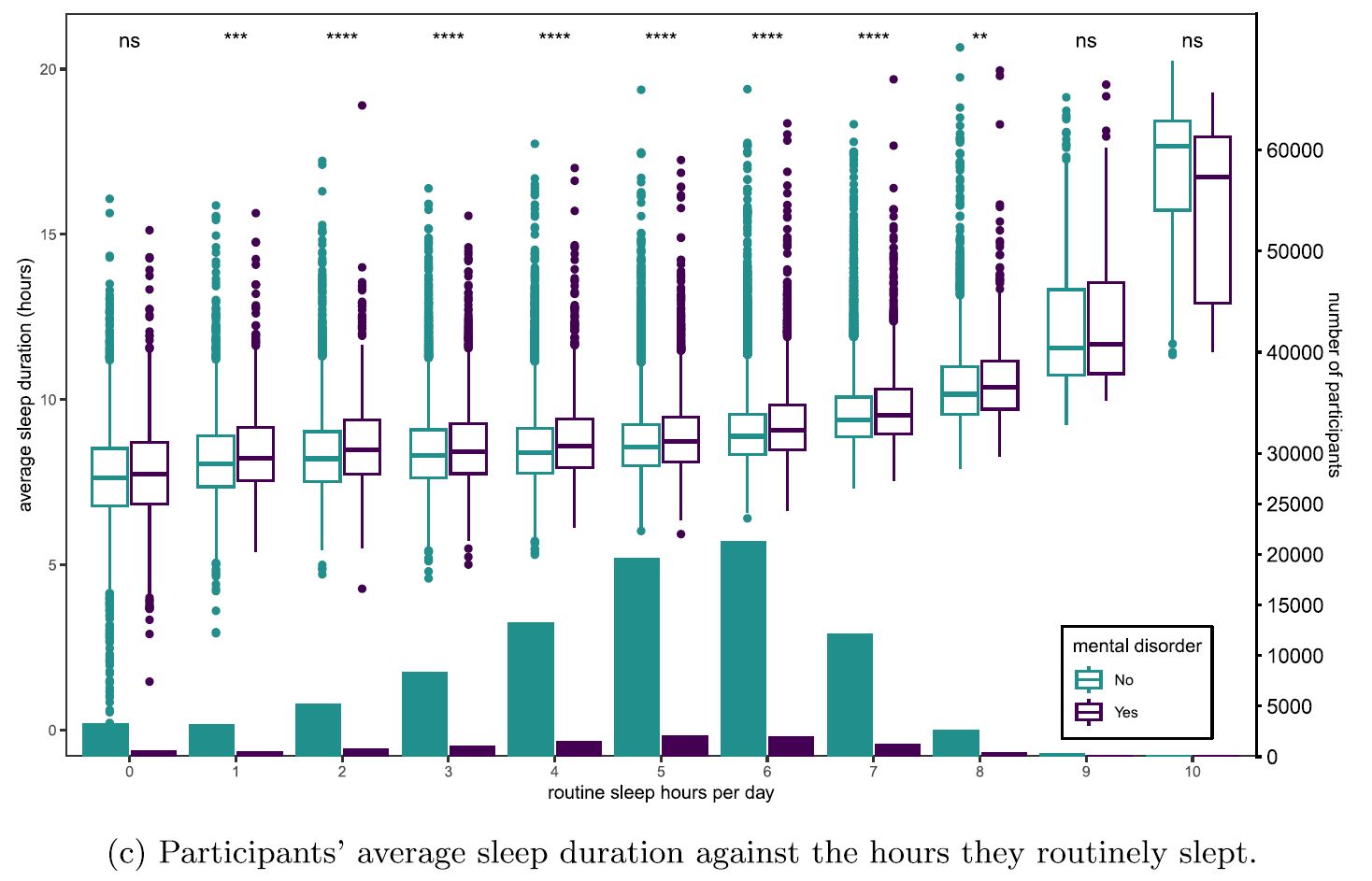
Figure 1. (c) Participants’ average sleep duration against the hours they routinely slept during the sleep behavior study, split according to prior diagnosis of a mental disorder. Differences in sleep duration per level of routine sleep hours depending on prior diagnosis: **** p ≤ 0.0001, *** p ≤ 0.001, ** p ≤ 0.01, ns p > 0.05 according to two-sided Wilcoxon signed rank tests. The secondary axis on the right is for the bottom histogram for each group.
Smooth 2D Interaction Effect Of Sleep Duration And Routine Sleep Hours
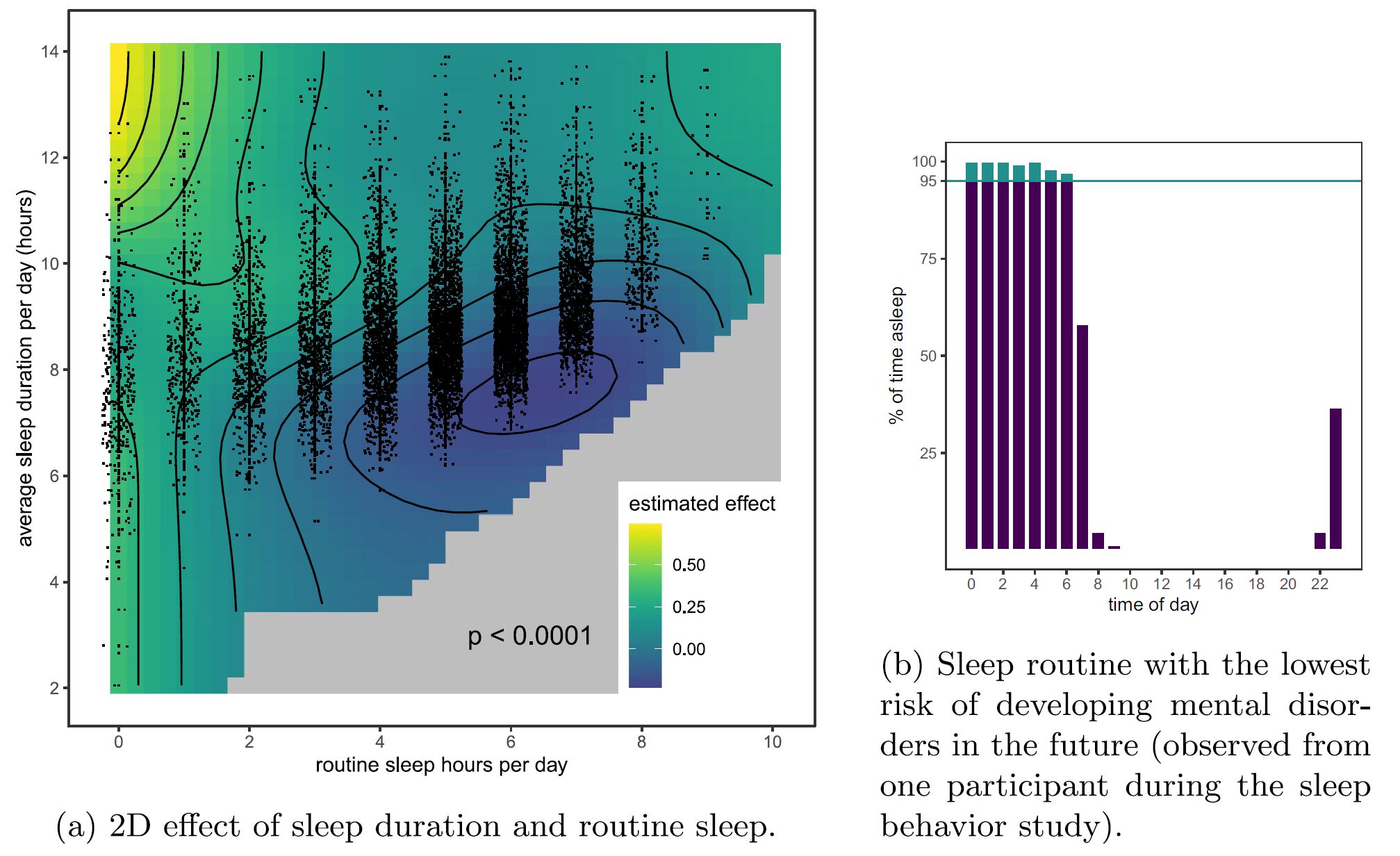
Figure 2. (a) The calculated 2D effect of average sleep duration and routine sleep hours on the hazard function of developing a mental disorder in the future (positive values increase the risk). Observed data points are presented as dots with jitter in the horizontal axis. Areas too far away from any data point are gray. (b) The observed sleep routine with the lowest risk of developing a mental disorder is 6 routine sleep hours at an average sleep duration of 6.8 hours.
Counterfactual Mental Disorder Incidence Rate Under Our Model

Figure 4. The probabilities of survival (i.e., the probability of not developing a mental disorder) per year are aggregated for all participants. We compare the calculated probabilities of not developing a mental disorder for all participants if they behaved as observed, and for the—according to our calculations— optimal but counterfactual case where all participants sleep for an average of 8 hours per day and for 7 hours routinely each day. (a) depicts the development of the whole 8-year follow-up. (b) shows the significant difference in survival probability after the 8-year follow-up (∗∗∗∗ : p< 0.0001 , two-sided Wilcoxon signed rank test)